The sloppy savior of humanity: how Alexander Fleming discovered penicillin (7 photos)
The Scottish microbiologist announced his world-changing achievement on September 30, 1928.
Author of the text: Aristarkh Konyukhov.
Material published in September 2021, partially updated in September 2023 
Alexander Fleming (1881-1955) Source: Mary Evans Picture Library via Legion Media
Who among us has not taken antibiotics? Medicines in ringing ampoules or shiny blisters have become an integral part of modern medicine. But before their appearance, people died from pneumonia, tuberculosis, and sometimes from a simple scratch, which could lead to blood poisoning. The spread of antibiotics began with penicillin, and the miracle cure was discovered - by accident - by Scotsman Alexander Fleming.
Shot of Fate
Alexander Fleming, the son of a Scottish farmer, did not dream of becoming a microbiologist. He moved to London at fourteen, lived with his older brother Tom, an ophthalmologist, and attended the Royal Polytechnic, where he studied business and commerce. After graduating from university at the age of 16, the future great scientist got a job at a shipping company, where after four years of work he realized that he did not want to do this. 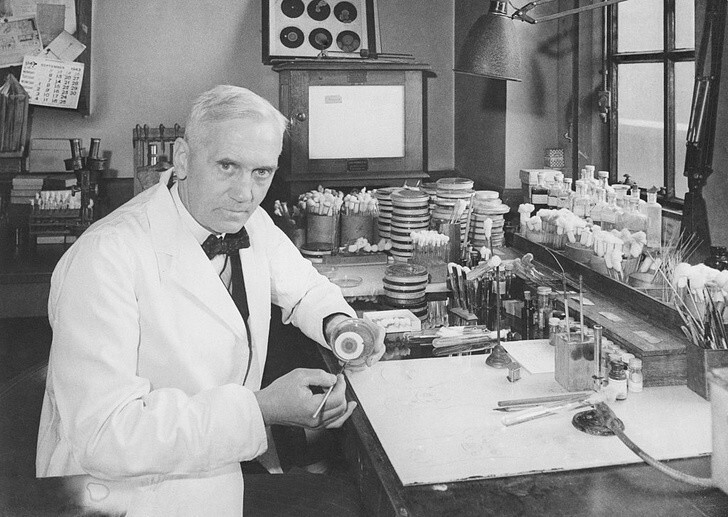
Alexander Fleming in the laboratory Source: Getty Images
Fleming started thinking about a medical career at the age of 20, deciding to follow the example of his successful brother. He had just received an inheritance from his uncle and used these funds to study at the medical school of St. Mary's Hospital in London's Paddington area, where he entered in 1903 at the age of 22. At that time, there were twelve educational institutions in London where Fleming could study medicine, but he dealt with the agony of choice radically: he remembered that he had once played as part of a water polo team against students from the school at St. Mary’s Hospital, and decided to go there. Three years later he received his bachelor's degree in medicine and passed the exams to become a surgeon.
So by 1906, Alexander Fleming had every chance to devote his life to surgery, only for this he would have to leave his native St. Mary’s Hospital, and fate had completely different plans for the young man.
Everything was decided by chance. The fact is that the young doctor, during his studies, was also a member of the shooting club, and the head of this club, Dr. John Freeman, really did not want to lose the talented shooter. Freeman then offered Fleming a job in the same research group at St. Mary's Hospital in which he worked. So Fleming became a student of Almroth Wright, a British immunologist and bacteriologist, creator of a vaccine against typhoid fever. 
Source: Getty Images
With the outbreak of World War I, Fleming joined the Royal Army Medical Corps and conducted a series of experiments that proved that antiseptics used to treat wounds do more harm than good, since they cannot destroy bacteria in deep wounds and reduce the body's actual resistance to infections by killing white blood cells. This was the first of the scientist’s serious discoveries.
The next one will happen in 1922. By this time, Fleming had already returned from the front to his home laboratory at St. Mary's Hospital. He devoted his work to the search for antibacterial drugs, having seen enough of the shocking deaths of soldiers from gangrene and sepsis at the front.
A talented scientist, Fleming was not distinguished by accuracy in his research, but his sloppiness only helped him. So, one day, coming to work with a cold, he sneezed into a Petri dish where he was growing bacteria, and discovered lysozyme, a natural antiseptic that can destroy the cell walls of some bacteria. Lysozyme, of course, was not a panacea and could not cope with serious diseases, but this was just the beginning.
Forgotten Petri dish
Fleming's sloppiness changed medicine six years after the discovery of lysozyme—but people didn't realize it right away. How did this happen?
The year was 1928. Alexander Fleming returned to the laboratory after a long vacation with his family and found forgotten Petri dishes with a culture of staphylococcus on the table. He conducted an audit and found out that some of the cups contained molds - and there were no bacteria around them at all! This alarmed the scientist. He concluded that the mold contained an antibacterial substance that killed staphylococcus, and spent the next days identifying the type of fungus that had found its way into the cups. 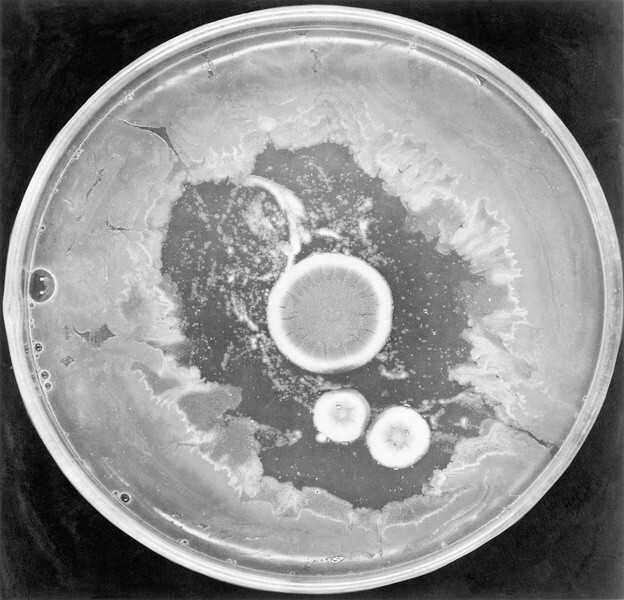
Source: Getty Images
Fungus Penicillium notatum deIt really has antibiotic properties, and the scientist named the active substance penicillin. During his research, Fleming found out that the drug is effective against staphylococcus, as well as the pathogens of scarlet fever, pneumonia, gonorrhea, meningitis and diphtheria.
Fleming presented his discovery to the scientific community in 1929: his article on penicillin was published in the British Journal of Experimental Pathology, but did not cause a strong reaction among his colleagues. Seven years later, he gave a presentation at the Second International Congress of Microbiologists in London, where he demonstrated his initial experience with Penicillium notatum and staphylococcus, but again no one supported the scientist’s opinion about the potential benefits of the discovered substance for treating infections in humans.
Confident that he was right, Fleming did not abandon the research, but extracting the active substance from mold, preparing it for long-term storage and producing the drug on an industrial scale turned out to be a real challenge, which the scientist was unable to cope with at that moment. Everything changed very soon.
Life-giving mold
It’s not that no one had thought about the anti-inflammatory properties of mold before Fleming. Moldy products were used to treat wounds in Ancient China, Ancient Egypt and the Inca Empire, and descriptions of the use of fungi for medicinal purposes are found in the works of Paracelsus and Avicenna.
Scientists of the 19th and 20th centuries also conducted research in this direction. Thus, the Frenchman Ernest Duchesne spoke at the Pasteur Institute in Paris with a report on the destructive effect of mold on the causative agent of typhoid fever, and the Americans Karl Alsberg and Otis Fisher Black, a year before the start of the First World War, were able to isolate an acid with an antimicrobial effect from the fungus. But these works did not receive recognition.
Penicillin and World War II
Penicillin owes its future not only to Alexander Fleming, but also to microbiologist Ernst Chain, who moved to Great Britain from Germany in 1933 due to the Nazis coming to power in their homeland. Chain got a job at Oxford University under Professor Howard Florey, where he began researching antibacterial substances. In particular, Cheyne was interested in one of Fleming's publications on penicillin, and he and Flory focused on this area. 
Source: Getty Images
In 1939, Chain was finally able to obtain a powdered preparation from the mold for subsequent research. Scientists decided to conduct a control experiment on mice: the rodents were infected with deadly bacteria, and those animals that received penicillin were able to survive. The main thing remained: to prove the effectiveness of the medicine for people.
The first intravenous injection of penicillin was given on February 12, 1941 to a London policeman suffering from blood poisoning. The results were impressive: the patient recovered and lived for another month, but died only because the allocated penicillin was not enough to completely defeat the disease. Scientists faced a new problem: it turned out to be impossible to organize mass production of the drug in Great Britain, which was subjected to constant bombing by Nazi Germany.
Realizing the complexity of the situation, the British turned to their American colleagues for help, and in the United States they managed to begin production of the first antibiotic. Then the need for it was already obvious: at the height of World War II, penicillin could save the lives of soldiers who were dying on the battlefield not so much from enemy fire as from infections that got into their wounds.
The Soviet Union also became interested in Fleming's discovery. Having not received the mold strain requested from Great Britain at the beginning of the war, the USSR began developing its own penicillin. This was carried out by a specially created laboratory of experimental medicine under the leadership of Professor Zinaida Ermolyeva. The first Soviet penicillin was isolated from the fungus Penicillium crustosum. 
Source: https://www.antibiotic.ru
In 1943, it was finally possible to establish production of the antibiotic in Britain, the drug began to be supplied to the army, successful tests of a drug for treating the wounded were carried out - penicillin received long-awaited recognition. Scientists threw all their efforts into research and production of the antibiotic: they looked for new strains of mold that could release more of the active substance. This is how Penicillium chrysogenum was discovered, from which they were able to obtain 400 times more penicillin than from the Penicillium notatum used by Fleming.
Soviet penicillin underwent a “baptism of fire” in 1944 - it was then that it entered military hospitals and began to be used to treat seriously wounded soldiers.
For nThe period of use of penicillin during the Second World War reduced the mortality rate from gangrene to zero in the Allied army, which was a significant advantage, because the losses of the enemy, deprived of access to the antibiotic, remained at the same level. After the war ended in 1945, Fleming, Chain and Florey were awarded the Nobel Prize for their research and discoveries.
What now
In 2028, penicillin will celebrate its hundredth birthday. During this time, several thousand new antibiotics were discovered, grouped into sixteen large classes. And penicillin itself, like its related drugs, is still used, only today it is suitable for treating a much narrower range of diseases than in its “golden” years. Why? Humanity is faced with a new problem, and its name is antibiotic-resistant bacteria. 
The Sloppy Savior of Mankind: How Alexander Fleming Discovered Penicillin Source: Getty Images
Over time, microorganisms mutate, adapting to the action of drugs, and acquire resistance. Alexander Fleming warned about this development of events: he argued that patients should not be administered penicillin in small doses for a short time. In other words, the course of treatment must be complete, and this applies not only to penicillin.
The fact is that in the body of a patient who takes antibiotics incorrectly, not all pathogenic microorganisms die - some of them survive, acquire resistance and infect new carriers. For example, some bacteria have “learned” to produce penicillinase, a special enzyme that breaks down penicillin and some other antibiotics.
We may not think about it, but the problem of bacterial resistance is becoming more and more acute: scientists note that recently microorganisms have adapted to antibiotics faster than humanity has time to find new ways to combat them.
It cannot be said that science is standing still in the search for new antibiotics: for example, in January 2015, the discovery of a new drug, teixobactin, was announced, which is effective against bacteria that have already developed resistance to other antimicrobial drugs. But it will take years before its widespread use, because after the discovery of the drug, all the necessary research must be carried out. In addition, teixobactin became the first new antibiotic in many years, and it is unknown how many bacteria managed to develop resistance during this time. Humanity simply cannot keep up with the rate of mutation of microorganisms, and we ourselves are worsening the situation by uncontrollably taking antibiotics.
So, almost a century ago, penicillin became the “magic wand” that turned deadly diseases into treatable ones, but will humanity cope with antibiotic-resistant bacteria? Perhaps we need another slob scientist who will leave a dirty Petri dish on the laboratory table?